When couples are trying for a baby they are full of questions – from how to maximise their chances of conception to how to relieve morning sickness and what cravings mean.
Whilst women tend to receive plenty of information from their healthcare provider, partners can be curious about the role they play in conception, how they can support their partner and how the body changes and adapts to pregnancy.
As many people turn to the internet to seek out information about conception and pregnancy, with the help of AI we sought out the most commonly searched questions on Google and other sources.
Women were more likely to ask questions about health and risks, and men asked questions about bonding with baby, supporting their partner and how they can be involved in pregnancy.
To uncover the most commonly asked questions, we used the advanced knowledge of ChatGPT to find the top 10 most searched questions by men, and by women, of which or inhouse team of registered midwives have answered with clinically accurate information on fertility, stages, sex positions and more!
Preconception
Results of our research shows that some of the top questions from women on the topic of preconception and getting pregnant were:
1. What are the best ways to prepare for pregnancy?
The best way to prepare for pregnancy is to become as healthy as possible. You can do this by:
- Breaking habits like smoking and drinking.
- Adopting a Mediterranean-style diet, with plenty of fruit and veg, healthy fats, whole grains, fish and seafood, some poultry and dairy, and limited amounts of red meat.
- Taking a good pre-conception supplement for at least 3 months before you start trying.
- Working towards a healthier weight, as being underweight or overweight can reduce your fertility.
- Reducing and learning to manage your stress levels.
- Learning about and decreasing the amount of toxins and pollutants you are exposed to (eg. in cleaning products, paints, plastics and pesticides)
- Exercising regularly.
- Reviewing any medication you may be taking, as some may affect fertility or be contraindicated in pregnancy).
2. How can I improve my fertility and increase my chances of getting pregnant?
- Eat a healthy and varied diet with plenty of fresh fruit and vegetables, healthy fats, whole grains, fish and seafood, some poultry and dairy and only limited amounts of red meat (similar to a Mediterranean diet).
- Cut back on processed foods, sugars, white flours, and foods high in trans fats, as all of these impact negatively on your hormone function.
- Have regular unprotected sex, every 2-3 days.
- Get to know your cervical mucus & chart your cycle, so you know when you are most fertile.
- Take a good quality pre-conception supplement of essential vitamins & minerals to boost your fertility and health.
- Stop smoking, drinking, and taking any drugs, as all of these can reduce fertility and harm your unborn baby.
- Reduce stressors wherever possible and learn to manage stress levels – nature, yoga, meditation, diet, exercise, and talking therapies can all help.
- Do regular exercise and work towards a healthier weight.
3. What lifestyle changes should I make before trying to conceive?
Give up smoking, drinking and drugs, as all of these impact negatively on your chances of conceiving and can harm your unborn baby.
Pay close attention to your diet and swap processed foods, sugars, and foods high in trans fats for plenty of fresh fruit and vegetables, healthy fats, wholegrain foods, fish and seafood. Have some poultry and dairy, and limited amounts of red meat.
Work towards a healthier weight, as women who are either underweight or overweight are more likely to not ovulate.
Stress affects your hormones and can lower your chances of conceiving. So, adopt healthy habits such as regular exercise and a healthy diet, give yoga and/or meditation a go, get out in nature and/or seek support from a professional to help lower your stress levels.
4. How long does it typically take to conceive?
Approximately 80% of women will conceive within the first 12 months of having unprotected regular sex. After this time, half of the women who have not yet fallen pregnant will go on to become pregnant in the following 12 months.
5. What can I do to manage stress during the preconception period?
– Connect with your mind and body through yoga and/or meditation.
– Get enough sleep.
– Engage in regular exercise.
– Eat a fresh and balanced diet.
– Plan some relaxation time with your partner – a day/weekend away, a massage, a spa day.
– Make relaxation time a ritual –a daily walk in nature, a regular movie night, late night swims at the local gym.
– Try to have fun and enjoy your relationship without fixating on becoming pregnant.
– Get to know your body, your cervical mucus, and chart your cycle – this will help you feel empowered and more relaxed.
– Consider seeking support from a counsellor, support group, mental health professional, or any other form of talking therapy.
– Continue – or start – to devote time to hobbies that make you happy.
6. Should I take prenatal vitamins before getting pregnant?
Alongside a healthy and balanced diet, taking a good quality pre-conception supplement will help ensure that you have optimal levels of essential vitamins and nutrients. These micronutrients, such as folate (the natural form of folic acid), vitamin D, iron, calcium, iodine, zinc and B vitamins, are necessary to help your baby develop and grow healthily, and to safeguard your wellbeing during pregnancy and the postnatal period.
Folate is naturally occurring – as opposed to folic acid, which is the man-made form of folate. Research shows that many of us have difficulty or are unable to metabolise (absorb and utilise) folic acid, which is of concern.
To ensure you have the optimal levels of folate for the healthy development of your unborn baby, look for a supplement that contains 400mcg of natural folate in the form of L-Methylfolate (5-MTHF), as well as 10mcg of vitamin D.
7. What are the risks associated with getting pregnant at an older age?
Most women over the age of 35 have healthy pregnancies and healthy babies. Yet, with increasing age, the chances of developing certain conditions and complications does slowly increase. These include:
– Pregnancy-induced hypertension (raised blood pressure)
– Gestational diabetes
– Problems with the placenta
– Down’s syndrome & other chromosomal abnormalities
– Miscarriage
8. What are the early signs and symptoms of pregnancy?
Every woman is an individual and, as such, their experience of early pregnancy may be quite different to others’. However, there are some early signs and symptoms of pregnancy that are most commonly experienced by women and these include:
– Having a missed period
– Period-type pains, or ‘cramps’
– Bleeding or ‘spotting’
– Breast tenderness and heaviness
– Needing to pass urine more often
– Fatigue and exhaustion
– Nausea
– Vomiting
– Strong sensitivity to smells
– Craving/rejecting certain foods
– Strange taste in your mouth
9. What are the most fertile days of my menstrual cycle?
Knowing the days you are most likely to be fertile can increase your chance of getting pregnant. Every woman’s menstrual cycle is different, so getting to know your body better can improve your chances of conception.
The average woman’s menstrual cycle lasts for 28 days, although some women will have shorter or longer ones, as we are all individuals. The most likely time an egg will be released during this time is approximately 14 days after the first day of your last period. This means that you will be most likely to conceive when you have regular sex around the midpoint of your cycle.
10. How can I track my ovulation and improve my chances of getting pregnant?
Monitoring vaginal discharge, your discharge continues to increase approaching ovulation, becoming looser and more elastic. When ovulation happens, the egg is released from the follicle in the ovary and is propelled into the fallopian tube, which is the place where fertilisation by sperm is most likely to occur.
Checking your luteinising hormone (LH), this peaks at around 24-36 hours prior to ovulation. So, detecting the LH surge in the menstrual cycle can help to identify the time of ovulation and the most fertile time during the menstrual cycle.
Monitoring basal body temperature (BBT) this can rise by around 0.5 degrees centigrade and stays raised until the body starts its period. Tracking your BBT can help you to understand possible patterns to your menstrual cycle and when it is most likely that you are ovulating each month.
11. What are the common causes of infertility in women and how can they be treated?
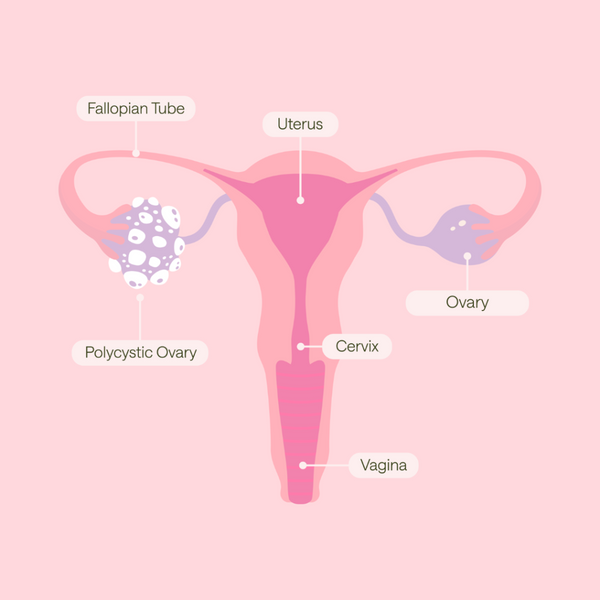
There are many possible causes of infertility and in a quarter of cases it is not possible to identify the cause. Common causes of infertility include: lack of regular ovulation or damaged fallopian tubes, endometriosis, where tissue that behaves like the lining of the womb is found outside the womb.
There are three main types of fertility treatment: Medicines, surgical procedures, assisted conception including intrauterine insemination (IUI) and in vitro fertilisation (IVF).
If you have a confirmed gynaecological diagnosis eg. polycystic ovaries or endometriosis you should seek a referral to a specialist for support with getting pregnant. Fertility treatment funded by the NHS varies across the UK. Waiting lists for treatment can be very long in some areas. The eligibility criteria can also vary. A GP will be able to advise about your eligibility for treatment.
12. What are the best sex positions for conception?
Studies have shown that no specific sex position increases the odds of getting pregnant. Sperm make their way to the cervix within seconds of ejaculation, no matter how the sex happens. Within 15 minutes, they can be found in the fallopian tubes, where your egg is (hopefully) waiting. That’s because sperm are extremely good swimmers, even when they’re swimming upstream against gravity.
13. How long should we try to conceive before seeking medical help?
Some people get pregnant instantly, but for others it can take longer. It's a good idea to see a GP if you have not conceived after a year of trying.
Women aged 36 and over, and anyone who's already aware they may have a confirmed gynaecological or fertility problem for example polycystic ovary syndrome (PCOS) or endometriosis, should see their GP sooner. They can check for common causes of fertility problems and suggest treatments that could help.
Infertility is usually only diagnosed when a couple have not managed to conceive after a year of trying.
There are two types of infertility, primary infertility, where someone who's never conceived a child in the past has difficulty conceiving or secondary infertility, where someone has had one or more pregnancies in the past, but is having difficulty conceiving again.
14. What are the common fertility treatments available to women?
There are three main types of fertility treatment:
- Medicines may be offered if you have ovulation problems, encouraging the monthly release of an egg (ovulation) in women who do not ovulate regularly or cannot ovulate at all.
- Surgical procedures, if your fallopian tubes have become blocked or scarred, surgery can be used to break up the scar tissue making it easier for eggs to pass through. The success of surgery will depend on the extent of the damage. Laparoscopic surgery is often used to treat endometriosis by destroying or removing fluid-filled sacs called cysts. It may also be used to remove fibroids. If you have polycystic ovary syndrome (PCOS), a minor surgical procedure called laparoscopic ovarian drilling can be used if ovulation medicine has not worked.
- Assisted conception - including intrauterine insemination (IUI) and in vitro fertilisation (IVF). If you or your partner has an infertility problem, you may be able to receive eggs or sperm from a donor to help you conceive. Treatment with donor eggs is usually done using IVF.
15. How can I prepare my body for a healthy pregnancy?
Our health and lifestyle have an undeniable effect on our fertility. Evidence shows that changing them can reverse their negative effects and significantly improve our chances of becoming pregnant. It is recommended that you should take a daily supplement (400 microgram) of folic acid (folate) every day before you get pregnant, and every day afterwards, up until you're 12 weeks pregnant. Folate is the natural form of vitamin B9, while folic acid is a synthetic form. Natural folate is more bioavailable than synthetic Folic Acid. This is especially important for the estimated 20%-60% of the population who have a variation in one of their MTHFR genes that negatively impacts their ability to convert folic acid (the synthetic version of B9), into the active form of folate.
Stop smoking. Smoking during pregnancy has been linked to a variety of health problems to you and your baby.
Cut out alcohol. Do not drink alcohol if you're pregnant or trying to get pregnant. Alcohol can be passed to your unborn baby.
Keep to a healthy weight. If you're overweight, you may have problems getting pregnant and fertility treatment is less likely to work.
Talk to a doctor if you have a long-term condition, such as epilepsy or diabetes, before you get pregnant, have a discussion with your specialist or a GP about getting pregnant.
And for men, some of the top questions around preconception were:
1. What lifestyle changes should I make before trying to conceive with my partner?
- Stop smoking. Smoking damages the DNA in sperm, resulting in reduced rates of conception and increased rates of miscarriage.
- Switch to a more Mediterranean diet – plenty of fresh fruit and vegetables, healthy fats, wholegrain foods, fish and seafood, some poultry and dairy, and limited red meat – and cut back on processed foods, sugar and foods high in trans fats.
- Keep your testicles cool and ‘loose’ by using loose fitting underwear and trousers, and by keeping the area away from direct heat.
- Drink within the recommended allowance (14 units/week) and spread this throughout the week – as opposed to ‘binging’.
- Reduce your exposure to harmful chemicals as much as possible (eg. in paints, glues, plastics, and food).
- Lower and manage your stress levels by engaging in regular exercise, eating a fresh and balanced diet, connecting with your mind and body through meditation and/or yoga, getting enough sleep, and seeking support from a counsellor, support group or mental health professional.
2. How can I improve my fertility and increase our chances of getting pregnant?
Men can improve their fertility by:
- Adopting a Mediterranean diet (shown to improve fertility), which includes plenty of fresh fruit and vegetables, healthy fats, wholegrain foods, fish and seafood, some poultry and dairy, limited amounts of red meat, and barely no processed foods, refined sugars, or trans fats.
- Working towards a healthier weight. Obesity is linked with fertility problems in men.
- Taking a good quality supplement that has been specifically developed to boost male fertility.
- Stopping smoking. Smoking damages the DNA in sperm, resulting in reduced rates of conception and increased rates of miscarriage.
- Keeping their testicles cool and ‘loose’ by using loose fitting underwear and trousers, and by keeping the area away from direct heat.
- Drinking within the recommended allowance (14 units/week) and spreading this throughout the week – as opposed to ‘binging’.
- Reducing exposure to harmful chemicals as much as possible (eg. in paints, glues, plastics, and food).
3. What are the common causes of male infertility and how can they be treated?
Male infertility may be caused by erectile dysfunction, ejaculation dysfunction, prostate problems, blocked tubes, low testosterone levels, or problems with the production and/or quality of the sperm.
Treatment will depend on the cause or causes of the infertility and may include:
- Medications - for erectile and ejaculatory dysfunctions, or low hormone levels
- Devices such as a vacuum pump if medication has not fully resolved an erectile dysfunction
- Surgery to remove blockages
- Or, if the above do not help, assisted reproduction techniques such as intracytoplasmic sperm injections (ICSI), in vitro fertilisation (IVF), intra-uterine insemination (IUI), or gamete intrafallopian transfer (GIFT).
4. How long does it typically take for a couple to conceive?
Every couple’s journey is different, and many factors come into play when they are trying to conceive, including the couple’s general and reproductive health, their lifestyle and stress levels, the woman’s age, and how often they have sex.
On average, in over 8 out of 10 of couples who engage in regular unprotected sex (every 2-3 days), the woman will become pregnant within 12 months. After this time, half of the women who have not yet fallen pregnant will go on to become pregnant in the following 12 months.
5. What can I do to reduce my partner's risk of miscarriage?
– Stop smoking – it can damage the DNA in the sperm and lead to miscarriage.
– Support her to stop smoking and drinking.
– Buy and prepare healthy foods for her/together – it’s easier to eat well if both of you do it.
– Support her in working towards a healthier weight, without criticism or pressure. Engage in regular exercise together, adopt healthier eating habits, and seek medical or therapeutic support to help her overcome any eating disorder.
– Avoid having certain foods in the house and, when out, remind her to stay away from:
- Unpasteurised milks & cheeses,
- Mould-ripened and soft blue cheeses,
- Undercooked eggs that do not have the Red Lion stamp,
- Undercooked or raw meats,
- Cold cured meats,
- Liver products,
- All kinds of pâté,
- Smoked fish that has not been cooked,
- Big fish like swordfish, marlin & shark,
- Raw shellfish.
6. Should I take any supplements or vitamins before trying to conceive?
Your nutrition is important in making sure that you and your sperm are in the best possible health to maximise your partner’s chances of getting pregnant and having a healthy pregnancy.
Alongside a healthy and balanced diet, you can help optimise your fertility and sexual function by taking a daily supplement containing the essential vitamins and minerals that are known to help sperm and male reproductive health. These include:
– zinc
– selenium
– Siberian Ginseng
– CoEnzyme Q10
– vitamin C
– vitamin D3
– vitamin E
– vitamin B6
– vitamin B12
7. What can I do to manage stress during the preconception period?
– Plan some relaxation time with your partner – a day/weekend away, a massage, a spa day.
– Make relaxation time a ritual –a daily walk in nature, a regular movie night, late night swims at the local gym.
– Try to have fun and enjoy your relationship without fixating on becoming pregnant.
– For some, it may work if the woman does not disclose when she is ovulating – this can reduce anxiety, which could lead to a partial or total loss of an erection, or an inability to ejaculate.
– Attend regular yoga and/or meditation classes.
– Eat healthily and engage in regular exercise.
– Consider a talking therapy.
8. What should I expect during a fertility evaluation and what tests will be done?
Your GP and/or fertility clinic will have a chat with you to find out about your medical history, your family history, and how long you and your partner have been trying to conceive for. They will then offer investigations to try and establish a cause for why a pregnancy has not occurred.
The most common tests include:
– A semen analysis to establish the health and motility of the sperm, as well as the sperm count.
– A urine sample to check for infection and retrograde ejaculation.
– Blood tests to check hormone levels, genetic conditions, and general health.
– Screening for sexually transmitted diseases, as some of these can directly impact fertility.
– An examination of the testicles to look for any lumps or deformities.
– An examination of the penis, to look at its shape, structure, and any potential abnormalities.
– An ultrasound scan of your testes.
9. How can I improve my sperm quality and increase our chances of getting pregnant?
About one in seven couples face issues with fertility, and in approximately 50% of cases, these are due to problems with male fertility. The first step to improving your fertility is to ensure you have a balanced and healthful diet with a healthy amount of exercise. The second is to supplement with vitamins, minerals and other nutrients that may be difficult to obtain from foods in the necessary amounts.
Reduction to alcohol consumption, stopping smoking and using illegal drugs, is advised. You should seek advice if you are taking certain medications, including testosterone replacement therapy, anabolic steroids, cancer medications (chemotherapy), some antibiotics and some antidepressants. If you are overweight or obese, weight loss may also be beneficial.
10. What is the role of a man in the process of trying to conceive?
Although a woman will be the one who technically gets pregnant, and carries and delivers the baby, a man also has a crucial role. For fertilisation to occur, his sperm must be healthy and strong to reach and penetrate the woman's egg. A man must be able to have and keep an erection, have enough sperm that are the right shape and move in the right way, and have enough semen to carry the sperm to the egg.
11. What are the best sex positions for conception?
Studies have shown that no specific sex position increases the odds of getting pregnant. Sperm make their way to the cervix within seconds of ejaculation, no matter how the sex happens. Within 15 minutes, they can be found in the fallopian tubes, the egg is (hopefully) waiting. That’s because sperm are extremely good swimmers, even when they’re swimming upstream against gravity.
12. What should I do if I have a low sperm count?
Your doctor may initially suggest trying to conceive naturally for a little longer. Many couples conceive within the second year of trying.
You can help maximise your chances of conceiving by:
- Having sex every two or three days.
- Moderating your alcohol consumption and stopping smoking.
- Staying in good shape, exercising regularly and having a healthy, balanced diet.
13. How long should we try to conceive before seeking medical help?
Some people get pregnant quickly, but for others it can take longer. It's a good idea to see a GP if your partner is not pregnant after a year of trying.
14. What are the common fertility treatments available to men?
- In vitro fertilisation (IVF) may be an option if you have a slightly low sperm count and you've been trying to conceive naturally with your partner for at least two years, an egg is removed from the woman's ovaries and fertilised with sperm in a laboratory. The fertilised egg is then returned to the woman's womb to grow and develop.
- Intracytoplasmic sperm injection (ICSI), in which a single sperm is injected directly into an egg to fertilise it. The fertilised egg is then transferred to the woman's womb.
- Donor insemination - using sperm donated by another man. You may wish to consider using donor insemination as an alternative to ICSI, particularly if you have a genetic disorder that could be passed on to any children. It can be used as part of IVF if necessary. If you're considering donor insemination, you should be offered counselling as a couple about the implications for you and your children.
- If you have very low levels of gonadotrophin hormones (that stimulate the production of sperm), you should be offered treatment with medicine to improve your fertility.
15. What can I do to support my partner during the process of trying to conceive?
Support can come in various forms. Something as simple as being engaged throughout the entire journey can go a long way. Being present throughout the entire process is one of the best ways to support your partner and there are various ways you can do this. Accompany her to doctor visits or check-ups, especially if they involve her receiving infertility treatment. She may be learning how to track her cycle, attempting to lose weight, or getting into the groove of eating healthy. Whatever it is, you can encourage her and show appreciation for the efforts she makes and join her in that journey.
If you and your partner have not conceived after trying for a long time, seeking a healthcare professional's advice is the best route to take. It should never, in any way, become a blame game, where one partner heaves the responsibility completely onto the other.
Don't ignore or neglect your emotions, keep yourself healthy, don't let trying to conceive overshadow everything else.
Pregnancy
We also asked Chat GPT for the most commonly asked questions around pregnancy from women and men:
Top 10 most commonly asked questions by women around pregnancy:
1. How can I confirm that I am pregnant?
Home pregnancy tests can be purchased in chemists and other shops as well as online and can be carried out from the first day of a missed period or from 21 days after unprotected sex. These tests are a simple stick which tests your urine. There are some extremely sensitive pregnancy tests available that can be used before you even miss a period, although it is worth noting that the pregnancy hormone hCG (human Chorionic Gonadotropin) may not be at detectable levels in the very early days of pregnancy, so a later test may be more accurate. HCG in the urine is often more concentrated in early morning samples during those early days, however as the hormone increases rapidly the longer it has been since a missed period the easier the hormone will be detected at any time of day by the test.
2. What are the early signs and symptoms of pregnancy?
The most common sign that can indicate you are pregnant is when your period doesn’t arrive. However, if your periods are irregular or fairly light this sign can be missed. It is unusual, but some women may continue to have regular periods whilst pregnant. Other common signs to look out for are sickness, nausea and tiredness, as this can occur from around 4-5 weeks of pregnancy. These symptoms can hit you at any time during the day or night and are caused by an increase in the pregnancy hormone hCG (human Chorionic Gonadotropin). Other common symptoms are sore and tender breasts, and increased awareness and aversion of smells and/or tastes, as well as craving certain foods or drinks.
3. What are the do's and don'ts during pregnancy?
It is good to listen to your instincts and body during pregnancy. Growing another human puts demands on you which are both physical and mental. The chances are there will be times when you feel more tired, sick or just generally drained, so take more time to rest and delegate to others if possible. Do try to continue to have regular physical activity, such as walking, swimming etc. as this will help maintain fitness levels for labour and recovery postpartum, although the first trimester you may want to ease off if you feel unwell. It is recommended not to smoke or drink alcohol during pregnancy and to eat a balanced and nutritious diet. Your midwife will recommend that you also take a supplement for Vitamin D and folic acid. Do ask your midwife about any concerns you may have regarding your pregnancy or baby’s wellbeing.
4. How can I alleviate morning sickness?
The most important things for pregnant women with morning sickness to do are listen to their body, rest as much as possible and try to eat and drink little and often as this will keep hydration levels up and help with energy.
There are also self-help remedies that you can try to reduce feelings of nausea and vomiting before using medicines or seeking medical help. Ginger is known for its anti-nausea properties. Pregnant women can try ginger in different forms to see if one type helps more than another. Examples include drinking hot water with chopped fresh ginger or eating crystallised ginger and ginger biscuits.
If pregnant women suffering with morning sickness can predict the times of the day when they tend to feel sick, eating something small, such as a biscuit or a bit of bread at this time, can help stave off those feelings. It may also help to avoid eating rich, creamy, or spicy foods, and stick to foods that are blander in smaller portions, rather than eating large meals.
5. What are the risks associated with pregnancy and how can I avoid them?
There are risks associated with pregnancy as the whole body is having to adapt to housing a growing baby and supporting its needs. Some medical conditions are linked to pregnancy, such as raised blood pressure (pre-eclampsia) and gestational diabetes. At your antenatal appointments, these complications will be discussed with you and further testing offered if you are at risk or show signs or symptoms of them. It is not just the physical risks which women should be aware of though, there are many hormonal changes which can affect mood and mental health. Women may develop low mood or mental health problems for the first time during pregnancy, but should also be made aware that if they have had prior mental health problems it may make them more susceptible to developing these again once they are pregnant.
6. How can I prepare for labour and delivery?
Antenatal classes have long been a source of information and a way to gain insight into understanding pregnancy and childbirth for women and their partners. The best time to start them is during the third trimester (after 28 weeks), as this will ensure that the information will be fresh in your and your birth partner’s minds as you approach your labour and birth. If you are well-informed about your options, you will feel more confident about making the right choices for yourself and your baby. Antenatal classes should cover key topics surrounding preparing for labour and birth such as perineal massage, colostrum harvesting and preparing for breastfeeding, as well as pain relief options, positions in labour, writing a birth plan and optimising your birthing environment.
7. How can I tell if my baby is developing normally?
Most women will be offered two ultrasound scans (USS) during their pregnancy. One around 8-14 weeks, which is when your pregnancy can be dated more accurately, and the other at around 20 weeks to check your baby’s anatomy for any problems.
Dating USS This is offered between 8-14 weeks of pregnancy as it can be easier to know how far along your pregnancy is, due to the distinct stages of development your baby is going through in the first trimester. It can also check that your baby is growing within your uterus and not in one of your fallopian tubes, as well as checking to see if there is more than one baby. Your baby is too small for any detailed checks of their anatomy to be done at this stage.
Anatomy USS At around 20 weeks of pregnancy, when your baby is bigger and their internal structures easier to visualise you will be offered an anatomy scan. This is to check their development, including: Spinal cord, brain, heart and other organs, as well as for cleft lip or palate, and can identify syndromes (such as Down’s, Edwards’ and Patau’s).
8. What are the different stages of pregnancy and what happens during each stage?
Pregnancy is often split into trimesters. The first trimester is from 0-12 weeks where conception and formation of their organs and bodies takes place. The second trimester is from 12-28 weeks where baby grows and develops further. The third trimester is from 28 weeks to the birth of the baby where they mature, lay down fat stores and their lungs mature in readiness for transferring to breathing in the outside world. A pregnancy is considered full-term at 37-42 weeks and if baby is born before 37 weeks they are premature and may need more input from the medical team.
9. What is a healthy pregnancy diet?
You need to eat a wide variety of foods in pregnancy so your baby can have access to the vitamins, minerals and nutrients necessary for optimal development and growth. It is important to ensure that you have enough folic acid (folate) for your baby to prevent neural tube defects such as spina bifida. Ideally, all women should take a supplement before and during pregnancy and try to eat a diet rich in folic acid (folate), such as granary bread, brown rice and leafy green vegetables.
A mixture of proteins, carbohydrates, fibre and healthy fats should be the basis of a balanced diet for you and your baby. Your midwife will be able to give you detailed dietary advice at your booking appointment.
10. How can I handle the emotional changes that come with pregnancy?
Changes in emotions and behaviour can hit hard during pregnancy, especially if it’s the first time someone has experienced this in their life. However, there is no need to suffer in silence hoping you will return to normal after the birth, you are not alone and it is very common to feel different or more emotional during pregnancy. Your midwife will have many resources she is able to signpost you to which you can use to help you cope with any emotional changes throughout pregnancy, so don’t be afraid to ask at your antenatal appointments for help.
Top 10 most commonly asked questions by men around pregnancy:
1. How can I support my partner during pregnancy?
There are a whole host of essential and practical jobs which need doing day to day so you can start by taking a larger share of the cleaning, cooking and shopping as needed. This could be in the early stages if she’s feeling more tired or experiencing sickness and nausea, or later on in pregnancy as bending and stretching become more difficult.
As pregnancy progresses become involved in learning how to support her during labour and birth as well as offering to massage her if she has sore feet, a stiff neck or back etc, she may even appreciate the offer of more personal care such as shaving her legs when she can’t reach or want you to help her do perineal massage. Don’t forget to support her emotional needs. Its common to have mood changes due to hormones in pregnancy and these can involve varied emotions! Be patient with her and tell her how proud you are that she is growing another human and reassure her that you still find her attractive.
2. What are the common health concerns during pregnancy and how can I help prevent them?
There are many common ailments during pregnancy which can’t necessarily be prevented but which you will be able to help her cope with. Sickness and nausea can impact upon day-to-day life in early pregnancy you can help by providing her with snacks and drinks rather than large meals. Keep away from creamy, rich or spicy foods. Later in pregnancy she may experience more aches and pains due to a growing bump, hormonal and posture changes. Offer to provide massage to the areas which need relief or run her a warm bath so she can relax her body and unwind.
3. What are the financial implications of having a baby?
Babies don’t need many things but the market is flooded with ‘must haves’. Research what will be helpful to you and within your own budget. You can ask friends and family what they found essential and what they didn’t find worth the money and why. One of the biggest financial hits will be to your income and adjusting to having less money once maternity pay reduces or if there are childcare costs when a parent returns to work after maternity leave. Not everyone plans a pregnancy but if you do, having some savings can be really helpful if a parent wanted to take more time off initially.
4. How can I prepare for the arrival of the baby?
The arrival of a new baby is a life-changing event. Learning about how to care for a newborn may sound scary but you will be surprised how soon you’ll learn how to do this. Antenatal classes can be invaluable for learning the basics surrounding newborn care, feeding, bathing etc. If your partner plans to breastfeed learning about how best to support them can be essential to their success, so choose an antenatal class package which covers this topic in detail.
5. What are the potential complications during labour and delivery and how can I be prepared?
The best way to prepare for labour and birth is to arm yourself with plenty of good-quality information. Antenatal classes, whether online, in person or on-demand, are a great way to help you understand and prepare for the realities of childbirth and what to expect once your baby arrives. Choose your classes carefully, midwife-run classes can be best, and make sure they cover the essential topics you need, which should include the following: pain relief in labour, induction of labour, and assisted and caesarean section births. Birth is unpredictable and understanding what to expect will help you to be able to support your partner well during the labour and birth, however things turn out.
6. What should I expect during prenatal appointments and how can I be involved?
Antenatal appointments start with the ‘booking in’ appointment. This usually happens at around eight to ten weeks. A detailed history will be taken, including family history and screening tests will be discussed - these involve blood tests and ultrasound scans. Midwife appointments will be offered every few weeks, becoming more frequent towards the end of pregnancy. Scans are offered at around 12 weeks to date the pregnancy and at 20 weeks to check anatomy in much more detail. Partners can be present at all appointments and this is a great time to ask any questions or to raise any concerns you may have about the pregnancy, birth or beyond, as your midwife will be able to signpost you to reliable sources for further information.
7. How can I bond with my unborn baby?
Being involved in the pregnancy such as participating in antenatal classes and antenatal appointments can help you feel more engaged and connected to your baby. You and your partner may want to discuss some time you can plan into your daily or weekly routines where you can talk or sing to your unborn baby - babies are able to hear and recognise voices and sounds from the 2nd trimester. Gentle massage during pregnancy can also help increase feelings of intimacy and connection between the two of you, if your partner feels like it, and also between you and your unborn baby. Another bonus is that couples who engage in pregnancy massage also report strengthening of their relationship.
8. How can I handle the emotional changes that my partner may be experiencing?
Your partner could feel proud and overjoyed, or scared, frightened and terrified, some may even be in denial that they really are pregnant, or a mixture of all of these feelings. The emotional impact of discovering you are pregnant can last days, weeks or longer. Pregnancy also creates considerable and sudden hormonal changes in the body, but emotions, mood and energy levels often start to improve after the 1st trimester. You can help her by being supportive and encouraging if she has any emotional changes, reassuring her that it’s normal. However, some women can have low mood which doesn’t improve, or gets worse. If you feel your partner is struggling, talk to her and encourage her to discuss this with her doctor or midwife who will have many resources, specific to your own locality, to signpost you both towards.
9. How can I help my partner manage stress during pregnancy?
Hormonal changes and heightened emotions can increase stress during pregnancy and often stress can impact on the physical and emotional wellbeing of both of you, so helping to reduce it will certainly be beneficial. You can help by encouraging her to do activities which help her to relax. If she has a busy lifestyle or you have other children help her to have time for herself by taking other children out, or picking up jobs to free up time for her to relax or do an activity of her choice. Talking honestly with your partner and asking her what would help her out the most can often reveal things you may not have previously thought of.
10. How can I prepare for the changes that will occur in our relationship after the baby arrives?
You can learn more about what to expect once baby has arrived by talking candidly with people who have experienced fatherhood. Men who have recently become fathers will give you an idea of how things may change. If you don’t know many or don’t want to ask there are plenty of new dads who have done podcasts on this subject, which can help you understand the changes and challenges which may be ahead.
Our team of registered midwives are always on hand to provide the latest news and advice on all pregnancy related topics, with a wealth of information available on the blog at myexpertmidwife.com.
Questions answered by:
Karen McEwen, Registered Midwife
Karen qualified as a midwife in 2007 and worked at teaching hospitals on delivery suites and birth centres for 12 years. She is experienced at supporting women having both low risk and more complicated births. She is also qualified to undertake the Newborn & Infant Physical Examination (NIPE).
Malena Monteverde, Registered Midwife
Malena Monteverde. Registered Midwife. Malena’s specialist areas are pregnancy, wellbeing & mindfulness, transition to parenthood, and breastfeeding. Malena qualified as an adult nurse in Oxford and then moved to Leeds to begin her midwifery training in 2001. She worked on Labour Ward for approximately 10 years and in the Community for another 7 years. She is training to become a Dru Yoga teacher and is also qualified to undertake the Newborn & Infant Physical Examination (NIPE).
Charlotte Hoskin, Registered Midwife and Advanced Nurse Practitioner
Charlotte has been a midwife for 15 years and nurse for 18 years, she continues to work clinically. Her specialist areas are intrapartum (labour ward / delivery suite) care, waterbirth, homebirth and prescribing in pregnancy. She is a mum of two, her first child was born on Channel 4 TV show, One Born every Minute, her second born at home, in water.