Constipation in pregnancy is a very common and uncomfortable symptom that can affect women throughout their pregnancies. It can bring other undesirable symptoms such as abdominal pain, backache, bloating, piles, general tiredness and even headaches.
Knowing how to manage constipation during pregnancy will significantly improve your wellbeing and quality of life.
What is pregnancy constipation?
Pregnancy constipation is the difficulty or, sometimes, temporary inability to pass a stool (have a poo) when you are pregnant. This may include not feeling the need to go, feeling like you need to open your bowels but are unable to, straining with little or no results, pain when you have a poo, and passing stools that are hard and difficult to part with. Constipation in pregnancy can be a ‘one-off’ episode, yet, for most women, it is a problem that they experience on and off whilst it becomes a chronic ailment for others.
Being constipated in pregnancy can be an uncomfortable experience, with many women reporting feeling ‘heavy’, bloated, ‘achey’ around their lower tummy and/or back, having an almost constant sensation that they need a poo, pain when they pass a stool, and increased tiredness.
When does constipation start in pregnancy?
For most pregnant women, constipation starts during their first trimester, usually after week 8, when the hormone progesterone steadily increases. However, every woman is an individual, and some women who experience constipation during pregnancy may not do so until their second or third trimester.
Causes of pregnancy constipation
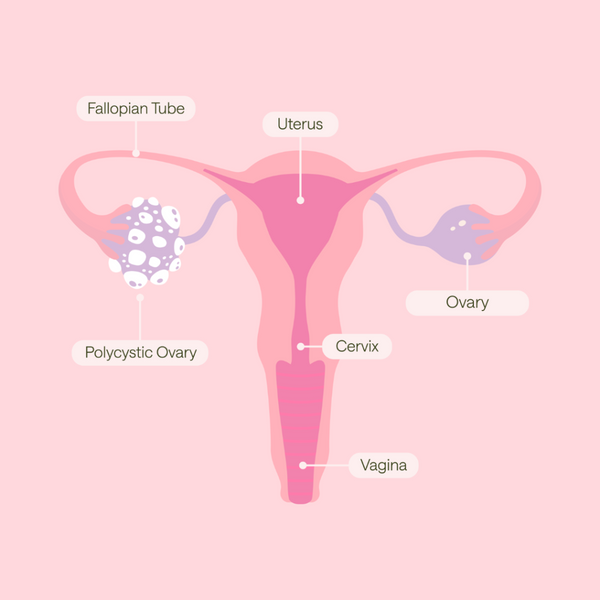
The hormone progesterone, essential in keeping your pregnancy safe during the first trimester, is responsible for constipation in pregnancy. But, whilst it is easy to blame many pregnancy ailments on hormones, pregnancy constipation can also be attributed to other causes, like your ever-growing uterus taking up space where your bowels would usually be, lack of adequate hydration and fibre intake, iron tablets, and diminished physical activity.
Hormones
The hormone progesterone - whose many jobs include protecting and supporting your early pregnancy - causes the muscles in your bowel, which move your stools along the intestine and out, to become lax, resulting in a slowing down of your digestive system. This affects your immediate digestion – leaving you feeling ‘full’ and more prone to ‘belching’ – and also your bowels, which take considerably longer to move digested food along it – resulting in increased gas, constipation and bloating.
Your growing womb
As your baby and womb grow, they take up essential space normally occupied by your bowel. This means your bowel has less room to go about its natural business. But your growing uterus also gets increasingly heavier, putting extra pressure on an already struggling bowel (think progesterone and lack of space), making it even harder for stools to move through and out of your body.
Inadequate hydration
When our body doesn’t get enough fluids, parts of it literally ‘dry up’. This is the case with your stools, which can become hard, dry and lumpy if you don’t drink enough.
Not enough fibre
Fibre makes your stools softer and easier to pass and provides ‘bulk’, which helps to keep your digestive system moving. If there isn’t enough fibre in your diet, your poo becomes harder, and your bowel struggles to move it along.
Reduced activity
Walking, running, cycling, swimming, yoga, etc., inadvertently massage our digestive tracts and help them work well. In pregnancy, tiredness, nausea, and other symptoms sometimes stop us from moving as much as we should, and this contributes to our gut becoming somewhat ‘stagnant’.
Iron tablets
Taking a supplement with the recommended daily allowance (RDA) of iron is unlikely to affect your bowels. However, iron tablets that have been prescribed by your doctor, or supplements containing higher quantities of iron, can often cause or worsen symptoms of constipation.
What are the symptoms?

As every pregnant woman is an individual, the symptoms of pregnancy constipation and the intensity of such symptoms won’t be the same for everyone. However, most women who experience constipation in pregnancy report many of the following symptoms:
Bowel Symptoms
Less frequent bowel movements – This is relative to what your habits are. If you usually open your bowels daily, you are likely to be constipated if you can only ‘go’ a few times a week.
Hard, dry and lumpy stools – Stools should be formed, smooth to pass and relatively soft.
Feeling like you need to go but can’t – The sensation is there, but it’s just not coming out.
Straining – This is a typical symptom of constipation and can be exhausting. It can also potentially lead to haemorrhoids (piles), anal fissures (small tears in/around your anus) and a weakened pelvic floor.
Bloating and increased wind – As your bowels take longer to move digested food, this creates increased gas and bloating.
Pain
Piles and anal fissures – Sitting on the loo for prolonged periods and straining can weaken your pelvic floor and increase pressure on the area, both of which can lead to swelling of the blood vessels around your anus – a.k.a. piles. Passing large, hard, dry and lumpy stools can damage the lining of your anus and cause tears – these are called anal fissures.
Pain when having a poo – This is usually caused by passing dry, lumpy and sometimes large stools, straining to pass them, and piles and/or fissures.
Pain/cramps in the lower abdomen are usually caused by increased/trapped gas, bloating, and the fact that hardened faecal matter (poo) is building up inside you and causing pressure and discomfort. Your midwife/maternity unit should always assess abdominal pain in pregnancy, so make sure to contact them even if you have other symptoms of constipation.
Lower back pain – This is usually described as a dull ache and is typically caused by stools ‘backing up’ in your intestines, which increases pressure on the surrounding area, including muscles and nerves. As with abdominal pain, it is best to be assessed to exclude other potential issues, such as a urine infection or pelvic girdle pain.

Other Symptoms
Tiredness and general malaise – This may be difficult to distinguish if you already feel tired during pregnancy. Yet, tiredness can be increased when you are constipated because your body is holding on to ‘toxic waste’. A sluggish digestive system and a full colon also make absorbing nutrients from food more difficult. You may also feel off food when constipated, exacerbating your tiredness and a general feeling of malaise. Make sure to see your midwife/doctor if you feel unwell or excessively/chronically tired, as these symptoms could also indicate other conditions, such as anaemia.
Headaches – Although the reasons for this are not clear; it is thought that straining, tiredness, dehydration and a build-up of toxins when you are constipated may lead to headaches. Headaches in pregnancy, although relatively common, should always be assessed by your maternity team as they could be a symptom of pre-eclampsia.
Pregnancy constipation relief

You will be pleased to know that there are several things you can do to help relieve pregnancy constipation and some of the symptoms associated with it:
Hydration
Drink up! - Increasing fluid intake by drinking more glasses of water daily and eating fresh fruit. Water ensures the smooth movement of solids through your bowel and helps to keep your stools soft, making them easier to pass. Warm liquids like hot water and lemon are particularly effective as they help to stimulate peristalsis (the wave-like motion that creates intestinal contractions), helping you go!

Exercise
Get moving - Exercise encourages bowel movements. Even something as simple as a brisk walk can help to get things moving. If any exercise seems too much (like it might for some women during their first trimester), listen to your body and rest. Try to do it mindfully when you walk or climb the stairs and engage your core. This will help your bowel movements.
Do your pelvic floor exercises – You may not see the connection, but maintaining a toned pelvic floor will push your stools out easier and prevent your pelvic floor from weakening, reducing the risk of piles and prolapse.
Massage your tummy - Abdominal massage can help relieve constipation, reduce discomfort and encourage regular bowel movements. It can be done lying, sitting or standing – so try a few different positions to find out what works best for you. You may want to use our Fantastic Skin Elastic, which contains grapefruit oil, known to help stimulate bowel movements. Learn how to massage your bump here.

Diet and nutrition
Pay attention to your fibre – For your bowels to work well, you need soluble and insoluble fibre. One will make your movements softer and easier to pass, and the other will add ‘bulk’ and keep your digestive system moving. Eating plenty of high-fibre foods is an easy way to increase fibre in your diet. Here are some good diet tips to follow:
- Add vegetables to meals
- Have porridge with berries and nuts
- Make soups and stews with barley or pulses
- Prepare smoothies with your favourite fruits
- Add prunes to desserts
- Change to wholemeal bread and pasta
Eat iron-rich foods – This will help you avoid needing iron supplements during pregnancy, which may cause/worsen pregnancy constipation. Have your iron-rich foods alongside some vitamin C (e.g. orange juice or a squeeze of lemon on your food) to help absorb iron, and avoid caffeine near meal times as this inhibits iron absorption.
Take your pregnancy supplements – Alongside an iron-rich diet, keeping your iron levels ‘topped up’ with a maintenance dose of iron will help prevent anaemia and, thus, the need for high-dose iron tablets. Choose a supplement that has been expertly developed, like My Expert Midwife’s Preconception + Pregnancy WOMAN*.

Other relievers
Elevate your feet – Did you know that squatting is the best position to poo in? Having your knees higher (ideally, higher than your hips) eases the passage of stools, reducing constipation, straining and piles. You can buy ‘purpose-built’ contraptions, but a high footstool, a sturdy box or a tower of Yellow Pages will also do nicely!
Talk to your midwife/doctor about taking stool softeners or laxatives – If lifestyle adaptations and diet don’t resolve your pregnancy constipation, seek medical advice about medication that will help and information about the types of laxatives. Stool softeners, like Lactulose, are usually safe to take during pregnancy, as are high-fibre drinks such as Fybogel, which helps by bulking your poo up with fluid, so it is softer.

My Expert Midwife is here to help you
Constipation is a common and uncomfortable ailment of pregnancy. Some of the many physiological adaptations of pregnancy are directly responsible for constipation, often from early pregnancy. The symptoms of constipation can vary in intensity and can negatively impact women’s quality of life and wellbeing during pregnancy.
Fortunately, many ways, including ‘home remedies and lifestyle adaptations, can help relieve constipation during pregnancy.
As well as staying hydrated, exercising and getting enough fibre, try taking good quality pregnancy supplements, enjoying an abdominal massage with Fantastic Skin Elastic, strengthening pelvic floor muscles and adopting a more ‘squat-like’ position for poo-ing.
And if you’re still struggling with constipation, seek medical advice and take laxatives that are safe for pregnancy.