Your pregnancy right up to the onset of labour is called the antenatal period (before birth). It is an important time which focuses on the health and wellbeing of both yourself and your baby, as well as planning for labour, birth, and the transition to parenthood.
This guide will tell you everything you need to know about antenatal care, including what to expect from your ANC appointments.
What is antenatal care?

Antenatal care is an umbrella term for every contact you have with a healthcare professional, from confirming your pregnancy through to established labour. That could be routine care with a healthcare professional or unscheduled appointments to discuss any concerns about your pregnancy as they arise, including but not limited to:
- Antenatal appointments with a community midwife
- Ultrasound scans
- Screening tests
- Antenatal clinic appointments
- Maternity assessment centre/triage visits
- Antenatal education classes
The purpose of antenatal care is to ensure the continued health and wellbeing of you and your baby and to act appropriately if any deviation from normal is identified.
When should I start antenatal care?

Antenatal care begins when you refer yourself for a booking appointment. Your referral will be risk assessed to ensure you begin on the right antenatal pathway, and you will then receive an invitation to attend an appointment either with your Community Midwife or with a Midwife based within the Antenatal Clinic at your hospital of choice.
You can usually expect a booking appointment at approximately 8-10 weeks of pregnancy based on the LMP (Last Menstrual Period) date you submitted in your referral. This gives time to organise time-critical screening tests, including booking blood tests and ultrasound scans.
You will attend routine appointments with your community midwife and only visit the hospital for scans and other screening tests. You can usually expect to meet with an obstetrician by 12 weeks of pregnancy.
If you are considered at higher risk:
- You may be invited to attend a booking appointment earlier, around 6-8 weeks based on your LMP.
- You may require shared midwifery/obstetric care. This means that you may attend some community midwifery appointments but will mostly be seen at the antenatal clinic by an obstetrician.
How do I get a midwife?
You may opt for either NHS or Independent Midwifery (IM) care throughout your pregnancy. Although, if you are anything other than low-risk, you will be advised to be seen by an obstetrician and any other specialist teams as appropriate.
If seeking an NHS midwife, you can either make a self-referral to the Trust of your choice or be referred by your GP. When registering with a midwife, your referral will be risk-assessed and assigned to a midwife, or a small team of midwives, depending on several factors:
- Who your GP is – most GP surgeries have an assigned midwife or team of midwives attached to them.
- Where you live – depending on your location, you may come under a specific midwife or team of midwives.
- Does your local Trust have Continuity of Care teams for those who may need additional support during pregnancy, such as teenagers, mental health, BAME (Black, Asian and Minority Ethnicities).
- Personal preference – you may have formed a relationship with a midwife or team of midwives during a previous pregnancy and would like to request the same carers. Please note: this may not always be possible, but the Trust will accommodate preferences where possible and appropriate.
If you have employed an Independent Midwife (IM), you should research who offers this service in your area and contact them directly. An excellent place to start is by asking family and friends for recommendations or seeking advice online.
Where will antenatal appointments take place?

Where your antenatal appointments take place will depend on whether you are suitable for midwifery-led care or require additional care from an obstetrician or other specialists during your pregnancy.
- Low-risk midwifery-led care appointments generally take place either at a GP surgery, a Children’s Centre or in your own home. However, this will vary from Trust to Trust.
- Independent Midwives (IMs) will usually organise all your appointments at home at a time to suit you and may be more flexible in their working hours.
- If you need to see an Obstetrician or any other specialist team during your pregnancy, this will usually be within the hospital, at an antenatal clinic or Maternity Assessment Centre.
- Screening tests such as Ultrasound Scans, Oral Glucose Tolerance Tests (OGTT) and Electronic Foetal Monitoring (EFM) will be conducted with the hospital as specialist equipment is needed. These health checks take longer and may require review by an obstetrician if there are any causes for concern.
How often will I see a midwife?
As antenatal care is tailored to your pregnancy and all pregnancies are individual, you may have a different antenatal appointment schedule from your friends, family or even compared to a previous pregnancy. This ensures you receive the right care for a healthy mum and baby.
First-time mums-to-be will tend to have slightly more appointments than someone who already has a child or children. However, you will also be offered more if you have a pre-existing condition or develop a condition during pregnancy that increases your risk factors.
What tests can I expect during antenatal care appointments?

From your first booking appointment, there will be screening tests discussed and offered to you to look for any health conditions that could affect either you or your baby.
Screening tests in pregnancy include:
Booking Blood Test
These are the blood tests that are offered at your first appointment with a midwife. The blood tests offered are:
- Hb (Haemoglobin) – the amount of red blood cells which carry oxygen around your body
- Blood Group – A, B ,AB, O
- Rhesus Status – positive or negative
- Infection Screen – including HIV, Syphilis and Hepatitis
- Thalassaemia and Sickle Cell disease – inherited blood disorders that cannot be cured but can be treated
- Antibody screening – to look for antibodies in your blood which could potentially attack your baby’s blood cells
Additional screening tests you will be offered include:
Combined Screening
- This is a blood test offered between 10-14 weeks of pregnancy which looks for markers in the blood for >Down’s Syndrome, Edwards’ Syndrome and Patau’s Syndrome.
- The results are combined with an extra measurement which can be taken at your Dating (12 week) ultrasound scan of a pad of fat on the back of the baby’s neck called the Nuchal Translucency (NT).
- The results of the blood test and NT measurement are used to calculate the chance of the baby having one or more of these genetic syndromes.
- It has an accuracy rate of approximately 90%.
Quadruple Screening
- This is a blood test which can be taken between 14-20 weeks of pregnancy, usually if you are too late for the Combined Screening or have declined Ultrasound Scans.
- This does not require an NT measurement.
- It only screens for Down’s Syndrome.
- It is less accurate at calculating the chance of the baby having Down’s Syndrome (75-80%).
NIPT (Non-Invasive Prenatal Testing)
- This is a blood test offered to all pregnant women privately or through the NHS to those women who have been identified as having a high chance of their baby being born with Down’s Syndrome, Edwards’ Syndrome or Patau’s Syndrome
- It has a 98% accuracy rate.
Dating Ultrasound Scan
- This is an external scan performed between 11-14 weeks of pregnancy by a sonographer within the hospital.
- The scan will confirm your EDD (Estimated Due Date)and the number of babies you are expecting:
- The sonographer will apply jelly to your abdomen and pass a probe over, the images will be seen in 2D black and white on a screen.
- The sonographer will take a lot of measurements of your baby or babies, which are then used to establish how many weeks and days pregnant you are and what your EDD will be.
- They will also look at where your baby is growing (that it is in the womb) and that it is developing as expected.
- You will also be offered a Nuchal Translucency measurement which forms part of the Combined Screening Test for Down’s Syndrome, Edwards’ Syndrome and Patau’s Syndrome.
- You should attend this scan with a full bladder to help the sonographer achieve better images of your baby.
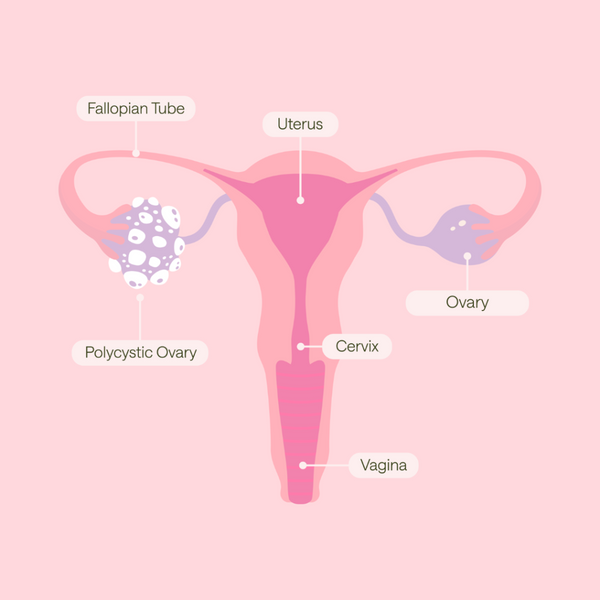
Fetal Rhesus Blood Test
- This is a blood test offered around 14-16 weeks of pregnancy, looking at something called cffDNA (cell free-fetal DNA).
- Genetic information from the baby which circulates in the mother’s bloodstream can indicate if a baby has a positive or negative rhesus factor.
- This test will be offered on the NHS to all women whose rhesus blood test indicates they are negative.
- The aim of the test is to identify which mums-to-be should be offered anti-d prophylaxis (rhesus-negative mum and rhesus-negative baby) injections to prevent complications associated with Rhesus Disease, a serious condition that can lead to anaemia and jaundice in babies often requiring treatment and extended hospital stays.
Urine Test
- This will be performed at every appointment you have with a midwife throughout your pregnancy.
- The main thing your midwife will be looking for is the presence of protein which later in pregnancy can be a sign that you could be developing a condition known as Pre-eclampsia.
- A urine test could also indicate that you have a urine infection or even be suggestive of diabetes if you repeatedly show high levels of glucose. Although this would need further controlled testing to be able to diagnose it.
- A simple urine dip can also tell your midwife if you are dehydrated and not drinking enough. Remember, you are more likely to become dehydrated in pregnancy as your body is placed under additional stress.
Blood Pressure (BP) Test
- A BP test will be performed at every appointment you have.
- A textbook BP reading is considered to be 120/80, but as this is an average, yours may be higher or lower and can be affected by stress, health, anxiety, fear, dehydration and activity.
- In pregnancy, the guidance is to maintain a BP of 140/90 or lower.
- If it appears that your BP is increasing and remaining consistently above this level, your midwife will refer you for a urine test and/or blood test which can confirm or rule out pre-eclampsia.
- If you are considered at high risk for developing pre-eclampsia, you will be offered a test between 20 and 36 weeks of pregnancy called PIGF (Placental Growth Factor). It is a blood test which indicates your risk of developing pre-eclampsia - low-risk, medium-risk or high-risk.
Oral Glucose Tolerance Test (OGTT)
- This test is offered to all women in some NHS Trusts and to women in higher-risk categories for developing Gestational Diabetes GDM), including women who have:
- Had GDM in a previous pregnancy
- A BMI higher than 30
- A first degree relative that has Type 1 or Type 2 Diabetes
- A previous baby weight with a weight above 4.5kg
- A family origin of South Asian, Black African, Black Caribbean and Middle Eastern descent
- You will also be offered this test if there is a suspicion from ultrasound scans that you have a higher than expected liquor volume (fluid around baby) or that baby has had a rapid increase in either estimated birthweight or abdominal circumference and falls out of expected range.
The OGTT involves:
- Fasting from the previous night (about 10 hours)
- A fasting blood test
- A measured glucose drink
- A 2 hour wait (you will be asked to sit down throughout to avoid using up glucose through exercise)
- A second blood test which will assess how your body has coped with the glucose over those 2 hours
You can then eat and drink normally. You will normally receive your results the same day.
Fetal Anomaly Ultrasound Scan (around 20 weeks)
- This is an external scan which produces a 2D black and white image on screen of your baby.
- The sonographer will take lots of measurements looking at the baby in fine detail including:
- The brain
- Limbs
- All four chambers of the heart
- Baby's organs
- Spinal cord
- Face and other structural feature
- This is a longer and more in-depth scan than the dating scan and you may be able to find out the gender of your baby at this scan if you want to (not always possible).
- You do not need a full bladder for this scan.
28 Week Blood Test
Your midwife will offer a repeat Haemoglobin test to ensure you have not developed anaemia during pregnancy, and a repeat blood group test to ensure we have the correct blood group on file for you.
Growth, Liquor Volume and Doppler Ultrasound Scans
This is an additional scan that you will be referred to if:
- You fall into a high-risk category for a small for gestational age baby (SGA)
- Your midwife is concerned about the growth of your baby
- You have expressed concerns about baby’s movements
A growth scan will estimate the baby's foetal weight and will give measurements of their head circumference, abdominal circumference and femur length.
- The results will indicate if there is any need for concern or further investigations.
- The aim of these additional scans is to identify babies at risk of compromise so that measures can be put in place to protect their health and wellbeing.
- These scans will also look at the volume of amniotic fluid around your baby and the blood flow through the umbilical cord between you and baby, both of which can indicate if there is a concern.
Foetal Heart Auscultation
- A Foetal Heart Auscultation is when a midwife can listen to your baby’s heartbeat using either a Pinard (a wooden, plastic or metal device) or a doppler which allows you to hear the heartbeat as well.
- This can normally be done from 16 weeks of pregnancy as this is when your baby has moved up above the pelvic brim making it easier to locate them.
- Never be tempted to try to listen in yourself. Midwives are trained for three years before qualifying and know how to use and interpret the doppler.
- It is very easy to listen to your own pulse, to get a doubling up of yours and baby’s heartbeat or to have other complications that a registered practitioner would identify as a concern but you would probably not, which could put your baby’s health at risk.
Electronic Foetal Monitoring
- This can be performed from 26 completed weeks of pregnancy (28 in some Trusts) and involves a midwife monitoring your baby on a CTG (Cardiotocography) for 20-60 minutes.
- 2 straps will be wrapped around your abdomen. The midwife will place a sensor which picks up waves from your baby’s heartbeat and a second sensor which assesses any uterine activity (contractions) under the straps to hold them securely in place.
- You will also be given a button to press which will leave a mark every time your baby moves.
- The pattern of the baby's heartbeat, combined with uterine activity and their movements gives us a big picture of how they are coping during pregnancy.
- It is likely that your midwife will also be using a computerised system called Dawes Redman which assesses the CTG throughout and comments on whether it is a normal or abnormal result compared with 1000s of previously stored CTGs of the same gestation.
How to prepare for antenatal appointments

Antenatal appointments are for the midwife or obstetrician to ensure a healthy pregnancy, and will involve the following:
- The offer of screening tests
- Lifestyle advice
- Mental health advice
- Sharing of evidence-based information about your pregnancy, birth and the postnatal period
- Baby care advice
- Advice on the transition to parenthood
But, just as importantly, it is a time for you to gather the information that you feel you need.
Being fully informed empowers you with knowledge when it comes time to make decisions about you and your baby. So, make sure you get the answers you need or ask where you can find them.

Other ways to prepare for antenatal appointments
Here are some tips to help you feel prepared for your antenatal appointments:
- Remember to take your handheld notes if you have them.
- Follow any specific instructions for the appointment, for example:
- Ahead of an OGTT, you must fast from the previous night.
- Ahead of a scan or blood test, you should be well hydrated.
- Try to organise childcare if you have other children. They may get bored waiting, and some Trusts do not allow children to attend, so always check beforehand.
- Take snacks and plenty to drink with you.
- Ensure your partner is free to attend.
- Take time off work – remember you are legally entitled to time off work to attend antenatal care appointments.
- Ensure you can get to your appointment:
- If you’re driving, do you know where to park? Have you got a parking disk or change for parking?
- If you’re catching public transport, do you know the times of your bus or train and where to get on and off?
Will I need to have any internal examinations?
It is unlikely that you will require an internal examination during your routine antenatal appointments. However, there may be occasions when a midwife or obstetrician will either recommend one or offer one.
These are the scenarios when an internal examination may be recommended:
- If a vaginal discharge suggestive of infection is reported – a vaginal swab which involves inserting a swab into the vagina (LVS – low vaginal swab or HVS high vaginal swab).
- If an early ultrasound scan (viability scan) is recommended for either poor obstetric history or vaginal bleeding. This may be performed TV (trans-vaginally), meaning a sterile probe will be inserted into the vagina to establish the cause of any vaginal bleeding and to look at the viability of the pregnancy.
- Towards the end of your pregnancy, you may be offered a membrane sweep (stretch and sweep). This is a vaginal examination performed by a midwife or an obstetrician where a gloved finger is placed inside the vagina to sweep the membranes of the amniotic sac surrounding the baby away from the cervix to try and stimulate the release of hormones (prostaglandins) which will soften and ripen the cervix making it more favourable for labour to start.
You can accept or decline vaginal examinations and should always be fully informed about the risks and benefits of the examination and why it is being advised or offered.
Feel prepared for pregnancy, labour and parenthood with antenatal education
An essential feature of antenatal care is your education. Be it your first or your seventh pregnancy, there may be information you are still seeking answers to, so attending antenatal classes is relevant to all pregnant people.
Do your research and find courses that suit your needs and wants, lifestyle and learning style. My Expert Midwife offers a series of on-demand online antenatal classes which cover 137 topics over 7.5 hours. Our antenatal classes are based on the most up-to-date evidence, written and presented by our in-house Registered Midwives, Consultant Obstetrician and Anaesthetist. Book onto our online antenatal classes here.